Ductus Arterioso Persistente (PDA) - Causas, Síntomas, Diagnóstico
Contenido
El conducto arterioso persistente es un defecto cardíaco congénito en el que el conducto arterioso sigue siendo funcional después del nacimiento.
Embriología
El conducto arterioso surge y se forma junto con la división del tronco arterial común. Durante la vida fetal, el conducto arterioso es una estructura normal que permite que la mayor parte de la sangre que sale del ventrículo derecho eluda la circulación pulmonar y pase a la aorta descendente. Normalmente, el conducto arterioso se cierra a los pocos días del nacimiento por falta de necesidad funcional.
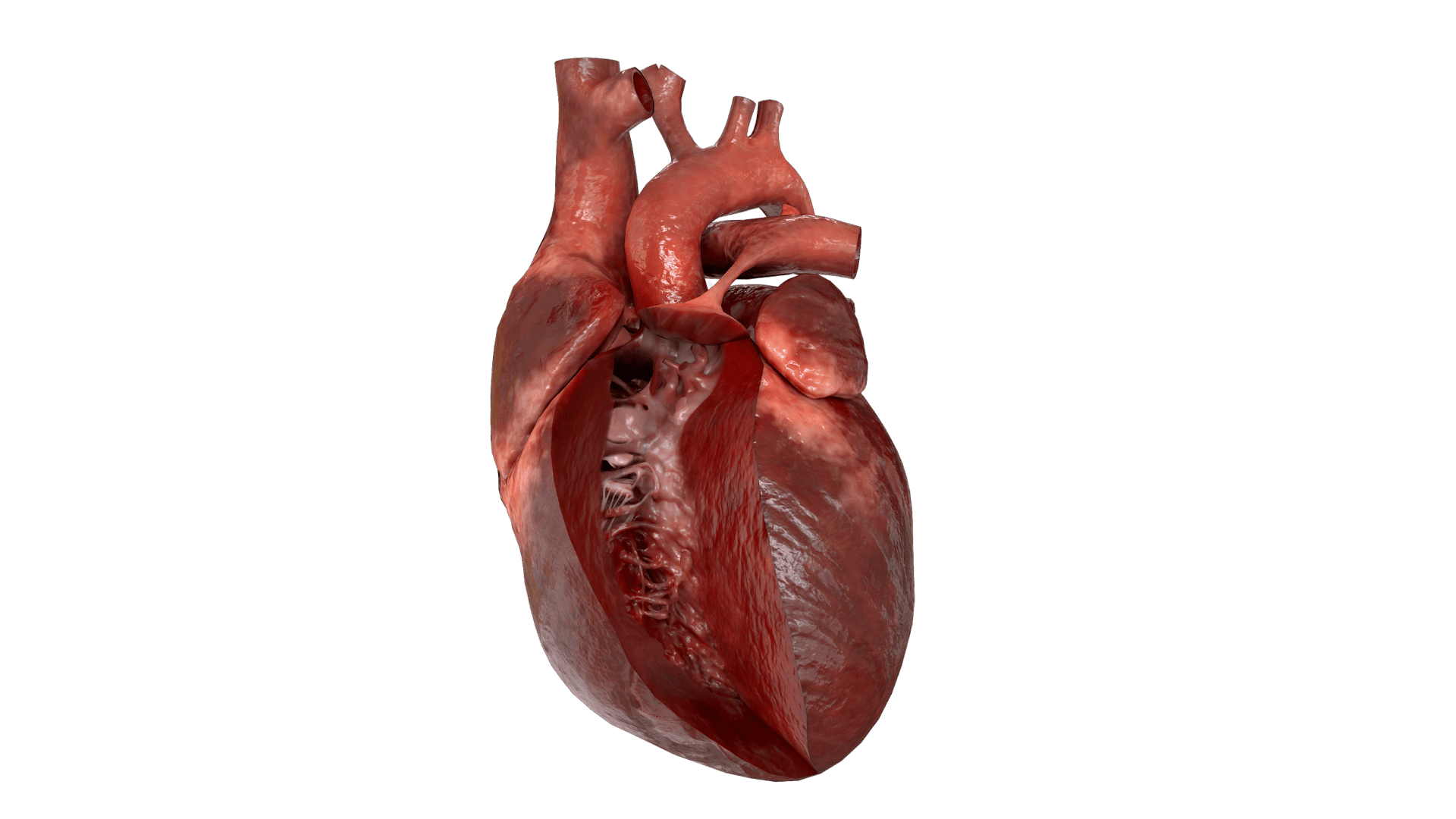
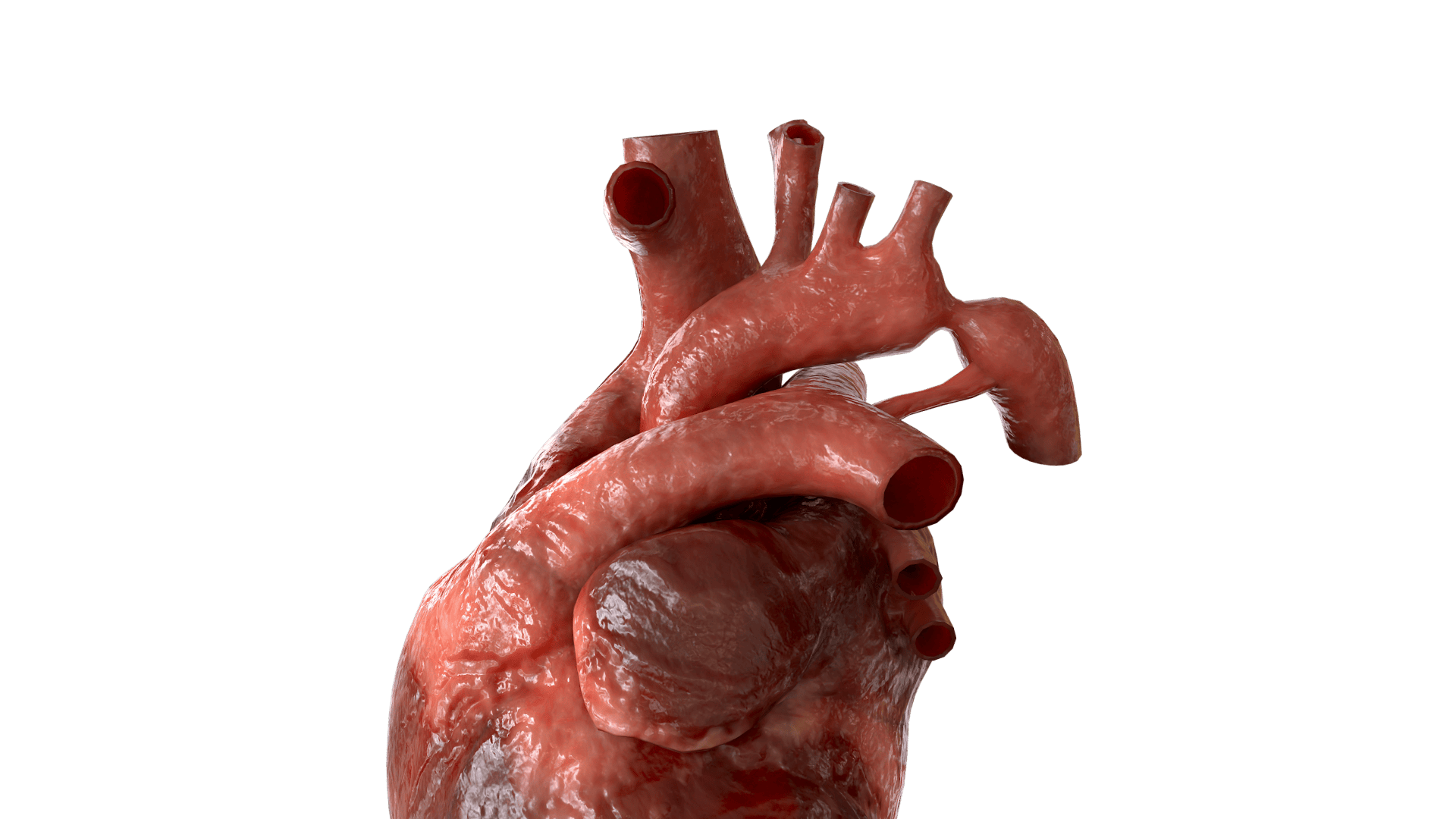
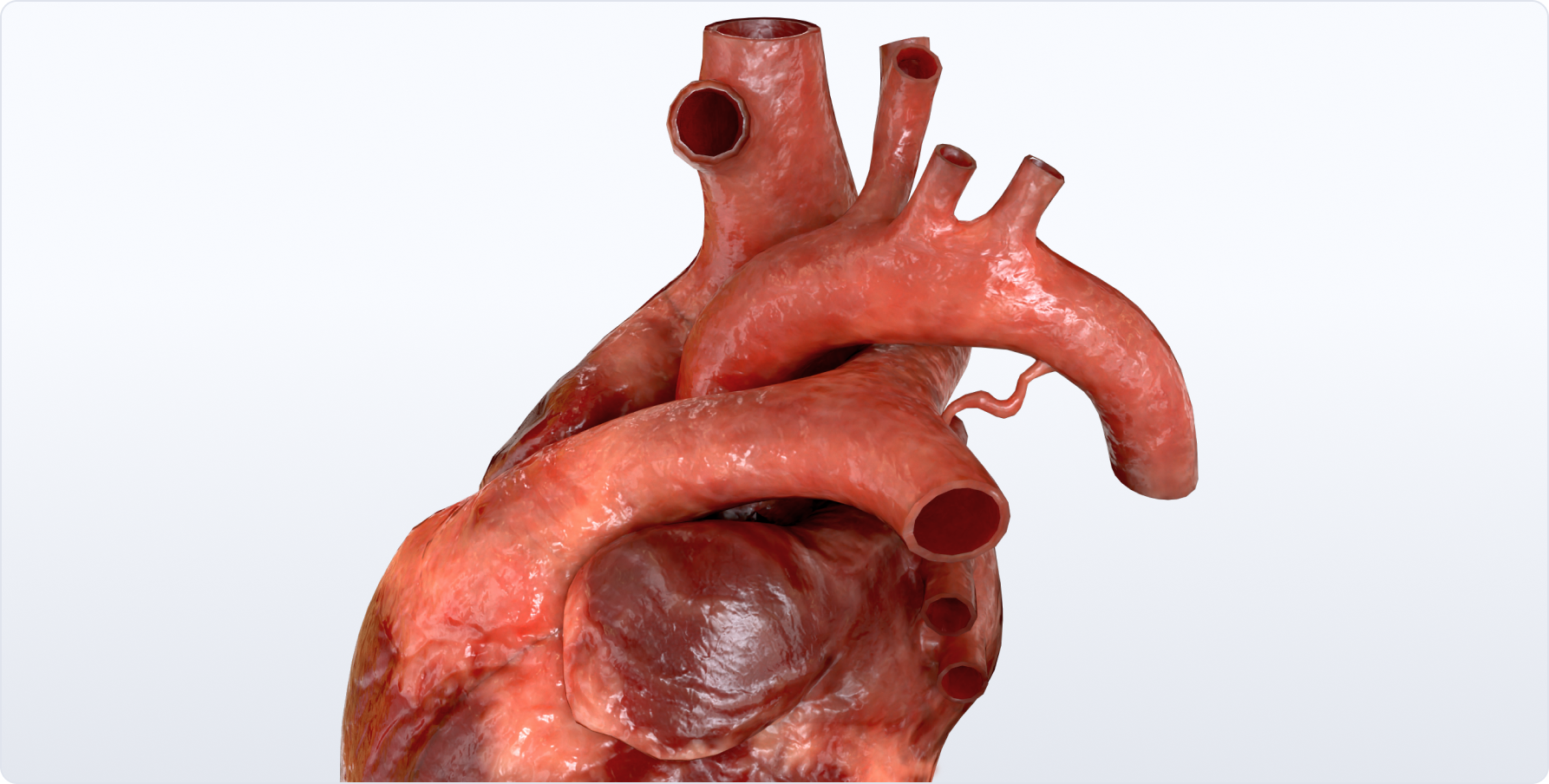
Anatomía
Lo más frecuente es que el conducto arterial parta de la aorta ligeramente por debajo de la arteria subclavia izquierda y se aproxime a la arteria pulmonar izquierda. Típicamente, el conducto tiene una forma cónica con un gran extremo aórtico que se estrecha hacia la pequeña conexión pulmonar.
Clasificación
Cónica;
Con forma de ventana;
Tubular.
Hemodinámica
La circulación sistémica se realiza principalmente a través del conducto arterioso: la sangre se desvía del sistema pulmonar no funcional a la aorta descendente. La primera respiración del recién nacido inicia el flujo de sangre hacia el sistema pulmonar. Con el tiempo, la resistencia de los vasos pulmonares disminuye, lo que provoca cambios en el flujo sanguíneo a través del conducto arterioso.
Un gran volumen de sangre pasa de la aorta a la arteria pulmonar bajo una gran presión. El mismo volumen de sangre regresa al corazón izquierdo, lo que provoca el agrandamiento de la aurícula izquierda y el ventrículo izquierdo. La magnitud del exceso de flujo sanguíneo pulmonar y la relación de la resistencia vascular pulmonar (RVP) con la resistencia vascular sistémica (RVS) (Qp : Qs) dependen del tamaño y la forma del conducto.
En última instancia, una sobrecirculación pulmonar constante conduce a la remodelación de la pared vascular y al desarrollo de la enfermedad obstructiva vascular pulmonar (EVOP). Tras un aumento significativo de la presión arterial pulmonar, la dirección de la derivación puede cambiar de derecha a izquierda.
Workup
Ecocardiografía Doppler, TC. Visualización y diagnóstico diferencial.
ECG. No tiene especificidad diagnóstica.
Radiografía. No específica. Los signos radiográficos de sobrecirculación pulmonar sólo se observan tras el desarrollo de hipertensión pulmonar.
Cateterismo cardíaco. Está indicado en casos de hipertensión pulmonar crítica para aclarar su naturaleza y las posibilidades de tratamiento quirúrgico.
Manifestaciones clínicas
Las manifestaciones clínicas dependen del tamaño del conducto y del estadio de los trastornos hemodinámicos. El niño típico con un conducto arterioso persistente es asintomático. Un conducto arterioso persistente de gran tamaño puede manifestarse en los primeros días de vida. Los signos clínicos típicos de insuficiencia cardiaca en estos niños serán: dificultad respiratoria, taquicardia, trastornos de la alimentación, hepatoesplenomegalia y retraso físico. También puede asociarse a infecciones respiratorias recurrentes, atelectasia e hipertensión pulmonar. Cuando cambia la dirección de la descarga sanguínea, la sangre arterial del arco aórtico expulsa la sangre venosa del conducto arterioso hacia la aorta descendente, lo que provoca principalmente cianosis en las extremidades inferiores.
Los signos típicos incluyen:
Soplo sistólico-diastólico continuo en el ІІ - ІІІ espacio intercostal a la izquierda del esternón;
Disminución de la presión arterial diastólica.
Tras la aparición de la hipertensión pulmonar, la naturaleza del ruido cambia: el componente diastólico del ruido disminuye y luego desaparece por completo.
Tratamiento
En los niños prematuros, se utiliza el tratamiento conservador del conducto arterioso persistente. Consiste en la administración de indometacina para obliterar el conducto. En la mayoría de los casos, está indicado el tratamiento quirúrgico. El tratamiento quirúrgico en recién nacidos está indicado de forma precoz para evitar complicaciones irreversibles del corazón y otros sistemas (los recién nacidos prematuros tienen muchas probabilidades de desarrollar ECN e insuficiencia renal). En caso de desarrollo de hipertensión pulmonar elevada con remodelación vascular pulmonar, el tratamiento quirúrgico está contraindicado.
Se utilizan las siguientes técnicas quirúrgicas:
Cierre del catéter;
Ligadura quirúrgica y/o clipaje que conlleva una toracotomía.
Fuentes externas
Catálogo VOKA.
https://catalog.voka.io/
Thapar, A., Jenkins, I. H., Mehta, A., & Davies, A. H. (2013). Diagnóstico y tratamiento de la aterosclerosis carotídea.
BMJ, 346, f1485. Doi: 10.1136/bmj.f1485
Goethem, J. V., Hatsukami, T., Rothwell, P., Brown, M. M., & Moody, A. R. (2021). Roadmap consensus on carotid artery plaque imaging and impact on therapy strategies and guidelines: An international, multispecialty, expert review and position statement.
Revista Americana de Neurorradiología, 42(9): 1566-1575. Doi: 10.3174/ajnr.A6798
Naylor, A. R., Ricco, J.-B., de Borst, G. J., Debus, S., de Haro, J., Halliday, A., ... & ESVS Guideline Review Group. (2018). Editor's Choice-Management of atherosclerotic carotid and vertebral artery disease: Guías de práctica clínica 2017 de la Sociedad Europea de Cirugía Vascular (ESVS).
Revista europea de cirugía vascular y endovascular, 55(1), 3-81. Doi: 10.1016/j.ejvs.2017.06.021
Moore, K. J., Sheedy, F. J., & Fisher, E. A. (2013). Los macrófagos en la aterosclerosis: Un equilibrio dinámico.
Nature Reviews Immunology, 13(10), 709-721. Doi: 10.1038/nri3520
Gracias por su comentario.
Tu comentario ha sido enviado a moderación y se publicará en breve. Le enviaremos un correo electrónico cuando esté disponible.